Ablation, or the use of high-frequency electromagnetic (EM) energy to destroy soft-tissue tumors, has been in existence for a few decades, but in recent years its underlying technology has evolved.
The benchmark of minimally invasive tissue treatment has long been the application of electrical current to kill abnormal tissues. This is done by heating tissues until they break down, a process called thermal ablation. Energy is delivered at 500 kHz, within the radio frequency (RF) range of the EM spectrum, hence these systems are called RF ablation systems.
In recent years, microwave (MW) ablation technology has also become commercially available and increasingly popular. At MW frequencies, oscillating EM fields are utilized to perform thermal ablation. Medtronic plc, Dublin, Ireland, one of the world’s premier medical technology and services companies, is a leader in both RF and microwave ablation technologies. With both RF and MW systems, the energy for ablation is applied using one or more needle-like probes.

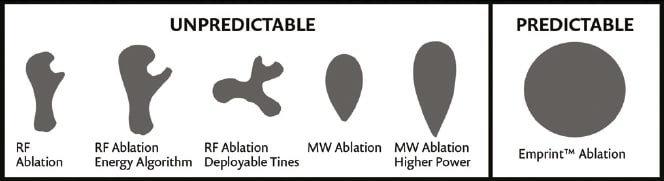
Medtronic’s latest innovation, the Emprint™ ablation system with Thermosphere™ technology, offers more predictable and repeatable results than other techniques and devices (See Figure 1). These advantages come from the fact that Thermosphere™ technology enables precise control of an EM field independent of the surrounding tissue environment.
Striving for Better Predictability
According to research, physicians rate predictability as their number one concern with ablation performance. The higher the level of predictability, the easier it is for a physician to plan a treatment procedure that will be safer, more effective, and less time-consuming.
Because of its nature, it’s challenging to be certain that RF ablation procedures will achieve the desired results. Given their different electrical conductivities, some tissues are less amenable to effective RF heating than others. Moreover, as the temperature in targeted tissue approaches 100°C, water in the tissue begins to vaporize and electrical conductivity rapidly decreases. This can make it difficult to generate temperatures high enough to cause cell breakdown.

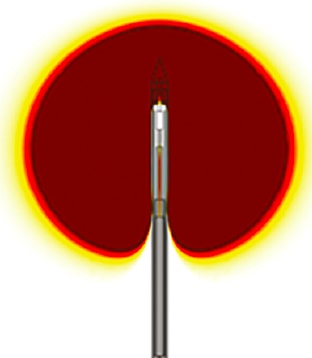
MW ablation technology attempts to overcome these limitations by using an EM field radiated into the tissue (See Figure 2). However, in practical application, tissue type and the vaporization of water during ablation cause the size and shape of the EM field to vary.
The Emprint™ ablation system with Thermosphere™ technology realizes the promise of predictability. It gives physicians the ability to easily control the thermal energy delivered by allowing precise control of the EM field across tissues and temperatures. This allows clinicians to accurately predict the boundaries and characteristics of the ablation zone.
Real-Time Monitoring of Ablations
“The challenge now is to monitor the ablation performance in real-time,” said Casey Ladtkow, principal engineer in the Early Technologies unit of Medtronic’s Minimally Invasive Therapies Group (MITG). “At present, when performing ablations, physicians don’t have continuous real-time feedback on the effectiveness of their procedure. If they could know exactly what is happening in real-time from start to finish, the effectiveness of ablation treatment would increase,” he said.
With some 40 staff members focused on interventional oncology, the mission of his unit is to deliver procedural solutions that alleviate pain, restore health, and extend life. Ladtkow and his team are using COMSOL Multiphysics® software to develop new ablation probes in order to achieve even higher levels of predictable performance and effectiveness.
One development-stage project is to optimize the design of these probes so they can both create a more precise ablation zone and also provide real-time feedback using radiometers.
Radiometers measure EM radiation and enable the characterization of the spatial distribution of an EM field. Ladtkow’s team is incorporating radiometers into Medtronic probes in order to give clinicians real-time feedback about the ablation zone. This will enable a clinician to fine-tune the zone as needed during the procedure, and to make sure the radiation destroys the targeted tissues while minimizing effects on the surrounding healthy tissue. (See Figure 2)
The team uses Multiphysics and its RF Module to help them model the probes and better understand and optimize their emitting/radiating and receiving/monitoring properties. “The performance and accuracy of MW ablation systems are affected by a number of dynamic factors that arise simultaneously in multiple physics domains. COMSOL software gives us the ability to perform the relevant complex modeling quickly and easily, to help us understand these coupled effects and improve our design,” Ladtkow said.
Simulation Enables Fast and Safe Design, Optimization, and Prototyping
For such a complex device, the traditional approach of building and evaluating a series of physical prototypes is all but out of the question because of the complexity and relationships among the many physics-based factors that impact device performance.
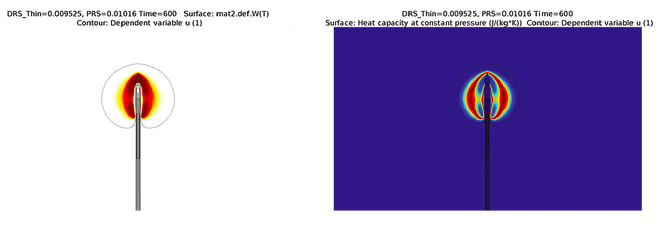
The team used the software to model the energy radiator and test designs that incorporated radiometric sensing in the same device. They simulated coupled thermal and electromagnetic effects around the radiative probe hardware to determine radiometric performance under different conditions (See Figure 3).
Ladtkow analyzed heat transfer in living tissue using a bioheat equation, which included a perfusion term, to account for blood flow cessation once the tissue coagulated (See Figure 4). This helped his team understand heat transport to cells around the tumor and predict the temperature distribution to ensure efficient and predictable energy delivery.
He performed other studies as well: investigations of temperature dependence of reaction rates (to understand the size of the ablation zone); radiometry modeling to determine how much energy enters the tissue and how much is reflected back into the radiator; and liquid-to-gas phase-change dynamics (See Figure 5). “The latter is critical to knowing what the wave pattern will look like, because knowing how much water is in the tissue is critical to knowing how a radiometer will behave, because of the change in wavelength,” he said.
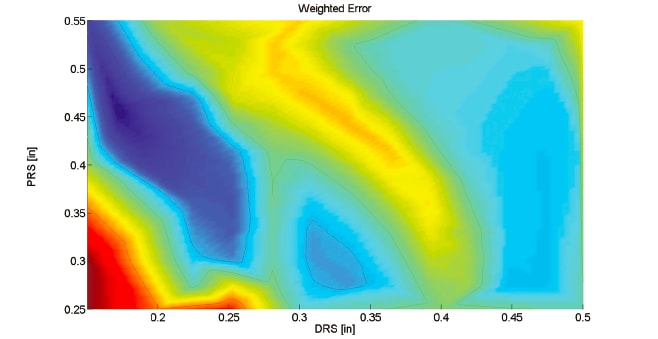
Simulation showed that lengthening the proximal radiating section (PRS) and shortening the distal radiating section (DRS) of an antenna would produce an efficient ablation radiator and an efficient receiver. These studies resulted in versions of a prototype ablation radiator with an integrated radiometer, along with results showing the performance of the integrated probe. (See Figure 6)
From Impossible to Possible
“Without COMSOL to help us perform these analyses, it simply would be impossible to do enough experiments to find an optimum solution that integrates an emitter and a receiver. COMSOL helps us see that certain architectures—which we’d never have investigated otherwise—might make an integrated device possible,” Ladtkow continued.
His team uses COMSOL software in conjunction with MATLAB ® software, and he said that the combination gives him a powerful ability to optimize complex models with highly sophisticated algorithms quickly and easily. He also hopes to integrate the Application Builder available in COMSOL Multiphysics into their modeling workflow. This would enable the team to create simulation apps allowing partners to test and verify different designs, while protecting their proprietary models.
“Based on our simulations, we are now realizing the potential to introduce ablation devices that will allow clinicians to not only deliver a precise energy dose, but also monitor ablations in real time,” Ladtkow said. “Multiphysics simulation enabled the rapid development, evaluation, and optimization of our design, which would not have been possible otherwise.”
This article was written by Valerio Marra, Technical Marketing Manager, COMSOL Inc., Burlington, MA. For more information, Click Here .



