At St. Jude Medical, ventricle assist devices are developed to improve the lives of patients with heart failure. Numerical simulation is used throughout the design process to characterize diverse concurrent aspects of the design, from thermal effects and fluid dynamics to power transfer.
The development of a device meant to assist or completely replace functioning of the heart is undeniably complex. This design process involves immense challenges, from supplying power to the device to ensuring that it does not interfere with normal biological functioning. Researchers at St. Jude Medical use multiphysics simulation to engineer left ventricular assist devices (LVADs) in an ongoing effort to improve the outlook and quality of life of patients with heart failure.
The condition typically begins with the left side of the heart, as the left ventricle is responsible for pumping oxygen-rich blood throughout the body, a greater distance than the right ventricle, which pumps blood through the lungs. Often, in patients with a poorly functioning left ventricle, an LVAD (see Figure 1) can provide mechanical circulatory support.
The ventricle assist device is the most complex machine ever implanted in a human being. An LVAD must circulate the entire human blood stream and support life, as well as be compatible with the internal environment of the human body. Thoratec, now part of St. Jude Medical, brought LVADs to a wide market in 2010, after years of clinical trials.
Designing a Powerful, Efficient, and Hemocompatible Pump
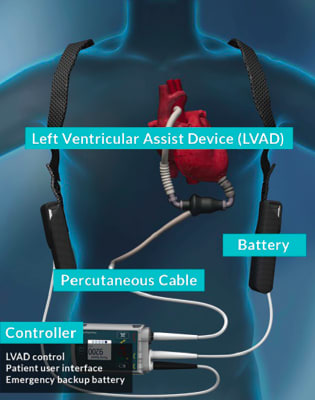
The design of an LVAD must take into consideration many factors. The device must be small enough to be connected to the heart and be made of compatible materials and geometry that permit the device to reside in the body without being rejected. Fluid dynamics, as well as thermal management and power supply, must also be considered. As multiple interacting physical effects must be accounted for at each area of development, multiphysics simulation is vital to the design process.
Freddy Hansen, senior R&D engineer at St. Jude Medical, uses his expertise in physics and mathematical modeling to characterize the system before experimental studies.
“I use COMSOL Multiphysics much like people used pocket calculators in the past. Some models are not too complicated. I can build one in a couple of hours and run it and get an answer. Others are quite sophisticated, and include CAD models with a lot of detail. I’ll work with some complex models for months before I’ve taken all of the information I want from them.”
Hansen began using COMSOL Multiphysics® software in 2011 and has since created upwards of 230 models that address a wide range of design challenges pertaining to the unique physics of artificial pumping devices.
With each generation of LVADs introduced to market, improvements are made that contribute to enhanced safety and quality of life for the patient. Research and development efforts at St. Jude Medical are centered on improving biocompatibility, hemocompatibility, and immunocompatibility, such that the device does not elicit an adverse immune response, nor interfere with other bodily systems. Numerical simulation is key to incorporating these considerations into the final design.
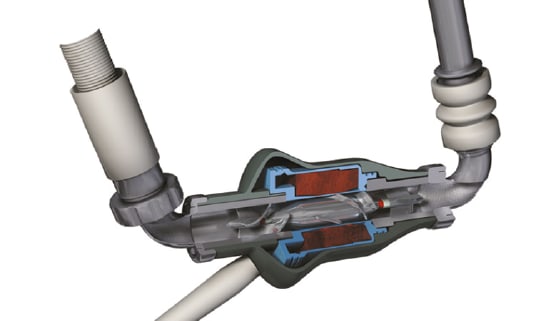
Geometry and size of the device play an important role in its overall effectiveness. To implant the LVAD, the surgeon connects one end of the LVAD to the left ventricle and the other end of the LVAD to the ascending aorta (see Figure 2). If the device is smaller, it is less cumbersome, and less likely to interfere with neighboring organs or tissue. Simulation allows for the evaluation of changes in size or geometry of the LVAD design before implementation in a physical prototype.
Optimizing LVAD Design for Biocompatibility
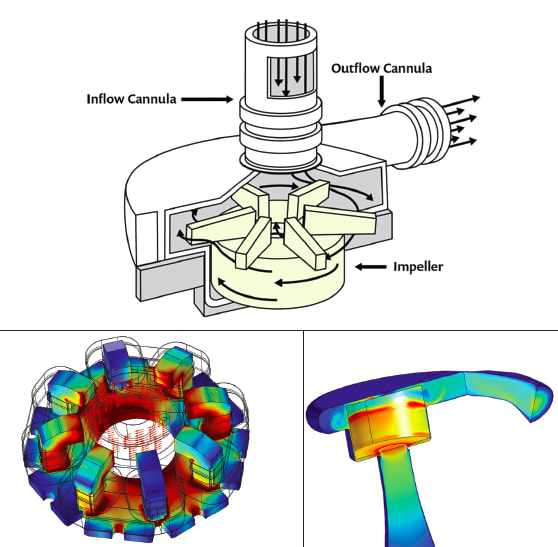
Many simulations were used in the development of the centrifugal pump of the LVAD. One challenge associated with engineering these devices is the prevention of blood clotting in any space in or around the pump. To address this, a magnetically levitated rotor was developed, which eliminated the need for ball bearings and other components with geometries that might promote clotting. Hansen used the rotating machinery modeling technology available in COMSOL Multiphysics to model both the magnetically levitated rotor and turbulent fluid flow.
A permanent magnet in the pump rotor is driven by 12 coils in the stator. The coils exert a torque on the rotor, as well as provide active control of the position of the rotor axis. The vertical position — or levitation — of the rotor is accomplished by magnetic field line tension and does not need active control. The rotor receives blood axially and redirects it radially, into the volute, or fluid collector (see Figure 3). Some of the blood backflows around the outer edge of the rotor and flows back into the rotor inlet, resulting in a constant washing of the blood, which serves to eliminate places where the blood can stagnate and clot.
Another significant advance was the development of a pump system with pulsatile flow, rather than continuous flow, which more closely mimics a functioning heart. The pulsatile flow aids in the washing of the blood, preventing blood clots, and is also believed to have a positive physiological effect on blood vessels throughout the body.
Wirelessly Powering a Fully Implantable LVAD
Current LVADs require power transfer from external batteries in a controller outside the body to the pump by way of a cable, for example, made with materials engineered to be biocompatible. But what if the cable could be eliminated?
Hansen explored transferring power by way of magnetic resonance coupling. Magnetic resonance coupling occurs when two objects having almost the same resonance frequency transfer energy to each other through their oscillating magnetic fields. In this way, power can be transferred from a power source to another device, even through a biological medium such as tissue.
A fully implantable LVAD system (FILVAS) would decrease infection risk and improve patient quality of life, because the patient would not need to be concerned with cable management. With this concept, the patient could shower or swim without concern for the cable.
To assess the feasibility of wireless power transfer to an LVAD and determine how power could be delivered between reasonably sized coils, Hansen coupled the simulation to a 3D magnetic field model and a 0D electrical circuit model to determine operating efficiency and power loss, as well as optimal circuit design and component values. He also used COMSOL to evaluate different materials for important components, such as the wires of the transformer coils, and to consider misalignment of a coil, the motions of coils due to patient walking, running, and doing other activities, and the presence of nearby magnetic or metallic objects. Hansen also used COMSOL to ensure that body temperature and biological systems would not be affected by the implant.
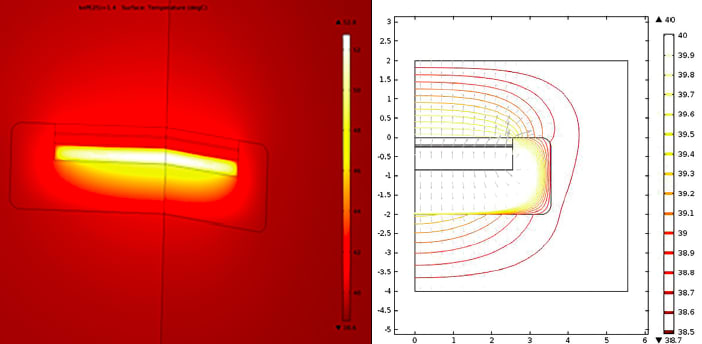
In order to accurately predict the effects of the heat flux emitted by a device, one must know or characterize the thermal properties for tissue. Hansen used COMSOL software to simulate a famous Cleveland Clinic experiment that characterized heat transfer from an implanted device through tissue.1 He used a parametric sweep in COMSOL to evaluate temperature throughout the tissue (Figure 4) for a range of thermal conductivity values.
He then compared the temperature distributions to experimental data from the Cleveland Clinic experiment to identify the thermal conductivity constant value that provided the best fit for the tissue. With this information, he could more accurately predict heat effects from the wireless transfer of power to an LVAD and use this information to ensure that the device would not cause an unsafe rise in body temperature.
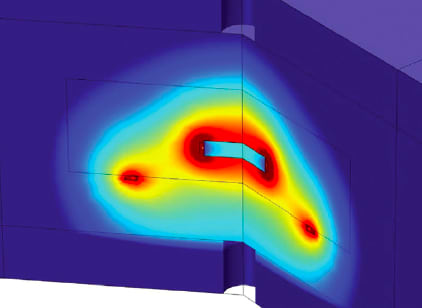
The wireless power transfer system induces small currents in the body tissue near the coils. Hansen modeled the heat generated in the tissue as a result of the induced currents (see Figure 5), combined this with models of heat generated inside the implant (in magnetic wires, electronics, and batteries), and then used the thermal conductivity coefficient that was determined from the simulated Cleveland Clinic study to determine the temperature in body tissue near the implant.
Protecting Life-Sustaining Batteries
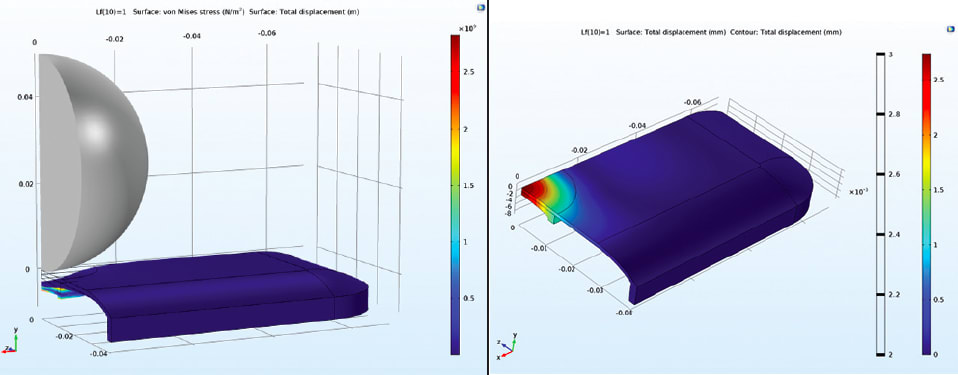
Hansen also used numerical simulation to develop the external components of an LVAD. Patients must live with their LVADs every single day, which inevitably means that the external LVAD controller must be able to withstand the wear and tear of life, as well as the occasional dropping of the controller to the floor. To ensure that the controller (which contains crucial life-saving batteries) will continue to function even if the patient tosses it around, Hansen developed a simulation in which a steel ball is dropped on the controller in order to assess its resilience.
Hansen compared the amount of mechanical energy necessary to deform the device with the known amount of kinetic energy in the steel ball at the moment of impact to determine whether the controller is sufficiently resilient. He also checked edges and surfaces of the deformed structural shell and frame for twisting that would imply that the controller would break. The analysis proved that the controller would continue to provide life-sustaining power to the LVAD even after a substantial impact.
New Technology Shows Improved Options for Patients in the Future
In designing devices to assist and replace the function of the heart, numerical simulation has proven to be essential. Hansen combines experimental characterization and mathematical modeling to thoroughly understand the physics of ventricle assist devices and improve the biocompatibility of the device as well as the overall patient experience.
The latest innovations to mechanical pumping systems — including a smaller device size, a more hemocompatible pump, the introduction of pulsatile flow, and now the possibility of wireless power transfer — hold much promise for better treatment in the future.
Reference
1. C. R. Davies et al., “Adaptation of Tissue to a Chronic Heat Load,” ASAIO Journal 40(3), p. M514-M517, 1994.
This article was written by Sarah Fields, technical marketing engineer for COMSOL, Burlington, MA. Freddy Hansen, Ph.D., is senior R&D engineer for St. Jude Medical, St. Paul, MN. For more information, click here .



