In the last three years, there has been an explosion of published content in medical journals related to 3D printing in medicine. This is a great testament to the uptick in innovation and application development around 3D printing and patient-specific 3D data, and how the combination of the two is changing how surgeries are being planned and performed, how implants are being designed and manufactured, and how mass customization for applications like hearing aids and dental aligners are going mainstream.

In 3D printing for healthcare, there is a shift in emphasis away from developing new printer technologies, and focusing instead on developing new printing materials as well as the digital software workflow used to create patient-specific digital content. Alongside these technology development trends, an abundance of application development for precision healthcare solutions is emerging, including patient-specific models, tools, and implants, with the solutions that have the least compliance burden migrating to the local hospital level.
It's All So Personal
3D technology is making waves in the healthcare industry by providing advanced tools for training, presurgical planning, and patient-specific solutions. Whether doctors are using unique 3D printed templates and guides for a surgery, or device companies are providing mass customized products to fit an individual's ear for hearing aids or bite for orthodontic aligners, 3D technology is a versatile and effective solution.
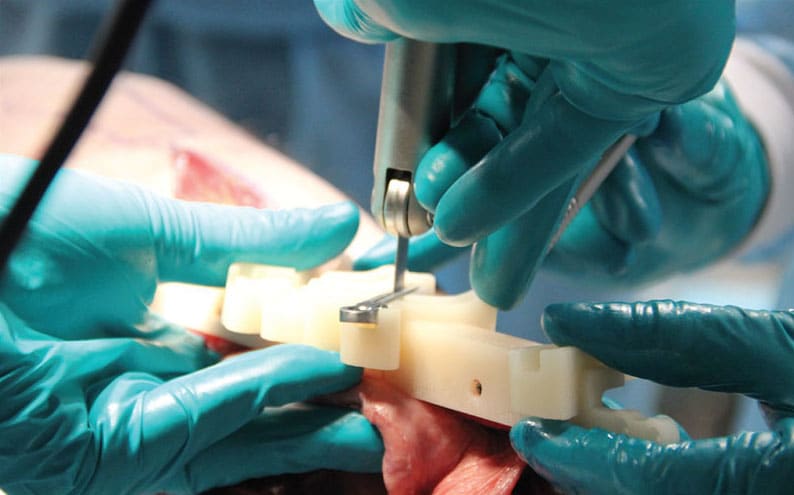
As one example, Virtual Surgical Planning (VSP), a service powered by a digital healthcare workflow, has been extremely helpful to doctors and surgical teams across the globe in preparing for rare and complex cases. By processing traditional 2D CT data into a 3D visualization, healthcare professionals can view, anticipate, and plan around difficulties or complications that may arise. These digital 3D models can be manipulated on screen to simulate surgical processes or brought off screen through 3D printing, all to help doctors solve the anatomical puzzle that's waiting for them in the operating room.
Presurgical knowledge of the cuts and movements that need to be made and the anatomical structures that need to be accommodated is valuable information that can help doctors save time, avoid surprises, and deliver successful patient outcomes. This capability gives surgical teams the opportunity to prepare for each patient better than ever before by essentially performing the surgery in advance. Patient-specific 3D printed anatomical models, guides, and templates can also be created in sterilizable and biocompatible materials for reference within the operating room, which is of further value.
Indeed, the use of digital solutions and 3D printing of patient-specific models, guides, and implants for rare and complex cases is one of the most impactful applications of 3D printing in healthcare to date. It truly helps to bridge any existing gaps in traditional surgical treatment to help deliver better patient outcomes.
Materials and Software
Materials and software are as important as the 3D printing technology. The 3D printing industry has needed to see the shift from 3D printing as a prototyping technology to a production technology for it to really go mainstream. 3D Systems’ new Figure 4 platform, for example, does just this. It is a modular, high-speed, production-ready system that allows for automation of the production workflow with precision and speed that will no doubt impact how medical devices are manufactured. In healthcare, it is exciting to see how such high-speed automated systems change the market, but what may be more interesting is the broad range of materials this platform can use for printing. Advancements in material development for platforms like Figure 4 and other production-ready systems for jetted and sintered materials will drive new applications in healthcare.
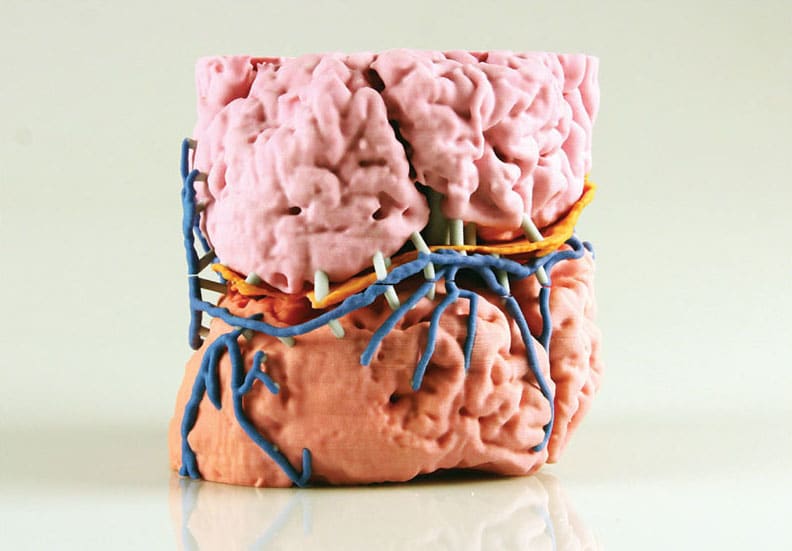
The industry is working continuously on developing new materials, specifically materials that are biomimetic. When printing a patient-specific anatomical model of a jaw deformity, that 3D printed model should act more like the actual bone of the human body. Similarly, if creating a patient-specific model of a congenital heart defect, it should provide the surgeon with a model of the heart that feels like a heart, can pump fluid like a heart, and responds like a heart to cuts or sutures. This will open up opportunities in advanced anatomical modeling and expand the use cases for 3D printed models from visual references to practice models for teaching, training, and presurgical simulation. This will also expand the library of available surgical simulation models by allowing lifelike models to be printed that represent complex and unique anatomies that are currently very difficult or rare to train on before a clinician sees his or her first case in the operating room.
As materials become biomimetic, they need to be biocompatible so they can be used in the operating room for short-term tissue contacting devices such as anatomical models, patient-specific guides, or disposable instruments, and even long-term implantable devices.
There has been a remarkable evolution in software over the last 10 years across precision healthcare applications. Many of these patient-specific healthcare solutions start with medical imaging data, and the image processing software involved has become substantially more efficient with the introduction of semi-automated processes. Surgical planning software also continues to evolve as major medical device companies, service centers, and startups all are developing applications around virtual surgical planning. Lastly, for patient-matched design applications such as bracing, CPAP masks, and surgical guides, more streamlined workflows for automated design of applications are becoming the standard to compete with the short turnaround time and low cost standards that are hitting the market.
Localization of Precision Healthcare Solutions


Anatomical models are the oldest use case for 3D printing in healthcare, going back to the late 1980s, and the pace of adoption in this application is finally accelerating. Hospital institutions are developing onsite print labs and bringing 3D technologies and expertise in house for more local and responsive solutions. For example, by pairing an image processing software like D2P™ (DICOM-to-Print) with a production-level 3D printer, it facilitates the creation of digital anatomical models using medical imaging data for applications ranging from visualization, to CAD, to 3D printing. Putting this capability into the hands of surgeons is a major advancement, especially when combined with other hardware, software, and service offerings. Whether clinicians are self-sufficient from start to finish, or whether their process is supplemented with ISO 13485 certified design and manufacturing facilities, localization enables a powerful, productive, and highly adaptable workflow.
These onsite hospital labs are generally set up centrally, and they are run in an autonomous manner to offer modeling solutions to as many surgeons and patients as possible. This has become a powerful evolution as localization of the technology to the hands of the users allows for new ideas and applications to emerge at a faster rate than can be done remotely.
Although this is an appealing concept, it does not come without challenges. First, there is still no insurance reimbursement in the United States for anatomical models (and virtual surgical planning), and this continues to pose challenges for adoption because it can end up forcing the hospital to absorb the cost. At a small scale this is sometimes done, but it is not a scalable practice. Although numerous peer reviewed medical journals are making various studied, backed, and repeatable claims of positive improvements with the use of anatomical models, there has been a lack of organization amongst institutions and industry to support nonbiased evidence-based trials. These types of trials, such as the 3DHEART trial, are finding momentum now and hope to pave the way for reimbursement. Reimbursement will drive the next wave of adoption.
As hospitals continue to adopt this digitization and manufacturing technology, they are becoming the legal manufacturer of these applications, which may be considered medical devices as defined by FDA. This is an evolving line that is currently getting some needed clarification in several journal articles, and the current understanding is that this determination is based on how much the anatomical model is altered from the imaging data before it is 3D printed. If the hospital is then becoming the legal manufacturer of a possible medical device, the question arises of how FDA will work to make sure patients are safe and applications are effective in an era of distributed, hospital-based manufacturing centers. The answer is still unknown. However, what is known is that hospitals will need to create rigorous quality management systems to ensure safety and effectiveness.
As these changes take place, we will see yet another surge in innovation, and surgeries will look very different in 10 years than they do now.
This article was written by Katie Weimer, VP of Healthcare, 3D Systems, Rock Hill, SC. For more information, Click Here .



