The most valuable innovations often arise when forward-thinking people see a problem in the world and then strive to create better solutions. That was the case for Derek Sham, founder and CEO of Cosm Medical, who — while working in the field of urology diagnostics — sought better ways of managing and treating pelvic floor disorders after watching his grandmother cope with pelvic organ prolapse. This common, painful, and stigmatized condition occurs when weakened or injured pelvic floor muscles or vaginal and connective tissues cause one or more of a patient’s pelvic organs to slip down from the correct position.
Physicians use a four-stage system to describe the severity of a patient’s pelvic prolapse. In the last stage, the organs are entirely out of the vaginal cavity. “When we found out she had prolapsed, she was already at stage 3 or stage 4,” Sham says. “And in my mind, that would not ever happen in a society where pelvic floor disorders are recognized as an issue.”
That lack of attention has led to countless women suffering in silence or enduring subpar interventions. Surgery is one option, but it is costly and often doesn’t yield permanent results.
The nonsurgical treatment is to use a pessary — a device inserted into the vagina to reduce prolapse and support pelvic tissues and organs or compress the urethra to stop urinary incontinence. Pessaries are one of the oldest documented medical devices and date back almost 4,000 years to 1850 BCE with the Egyptians. After the advent of medical-grade silicone, pessaries have remained largely unchanged for the past 50 years. Fit for patients by doctors through clinical experience and trial and error, pessaries come in more than 100 different shapes and sizes.1
Sham knew there was a better way. “There are 100 different pessaries because every woman is different,” Sham says. “It’s really about modernizing care by bringing precision and personalization to make a difference in each woman’s life who wears these devices, because over 10 million pessaries are sold globally each year. About a third of women currently fail the fitting process; half will stop using them within a year or two; and over half get complications with long-term use.” Complications for pessary use include chronic pain, bleeding, constipation, urinary obstruction, infections, and tissue abrasion.2
A Prevalent Issue
Pelvic floor disorders are not an everyday conversation topic, but they are more prevalent than people realize. “They affect one out of four women of all ages — one out of three over 60 and one out of two over 80,” says Cosm medical chief scientific officer Goli Ameri. “Given the aging population, you can get a grasp of what a big problem it is now and how much of a bigger problem it will be in the future. In 2020, adult diaper sales for the first time in history surpassed baby diaper sales in North America.”3
Patients experiencing prolapse appreciate the ability to maintain autonomy for their medical needs. However, that’s often not an option with conventional pessaries. “Over half of women can’t self-manage their pessaries because current designs can be painful to insert and remove, and some patients don’t have the finger dexterity or the capability to reach that far into their vagina,” Sham says. His goal is to get rid of the trial-and-error fitting process and make pessaries personalized and much more user-friendly: something that can be handled without help — as simple as wearing a bra — that is put in at the start of the day and removed to sleep.
Patients who have difficulty inserting and removing conventional pessaries currently must return to clinics every three to six months to have the devices cleaned and let doctors check the health of their vaginal tissues. “We will help some of those women to self-manage their devices to improve autonomy and quality of life while lowering risk of complications,” Sham says. “Many women end up going to nursing homes because of either the burden, discomfort, and pain from prolapse or incontinence that they can’t manage at home.”
Custom Solutions
Custom-made medical accessories are already widely used for other conditions, such as in orthotics, hearing, and dental. Cosm Medical uses customization and artificial intelligence (AI) to create made-to-order gynecological prosthetics it calls Gynethotics™, custom pessaries that lower risks and enhance care for patients with pelvic floor problems. Cosm Medical is part of the Autodesk Technology Centers Outsight Network, which has provided the team tools and support to help develop its novel system.
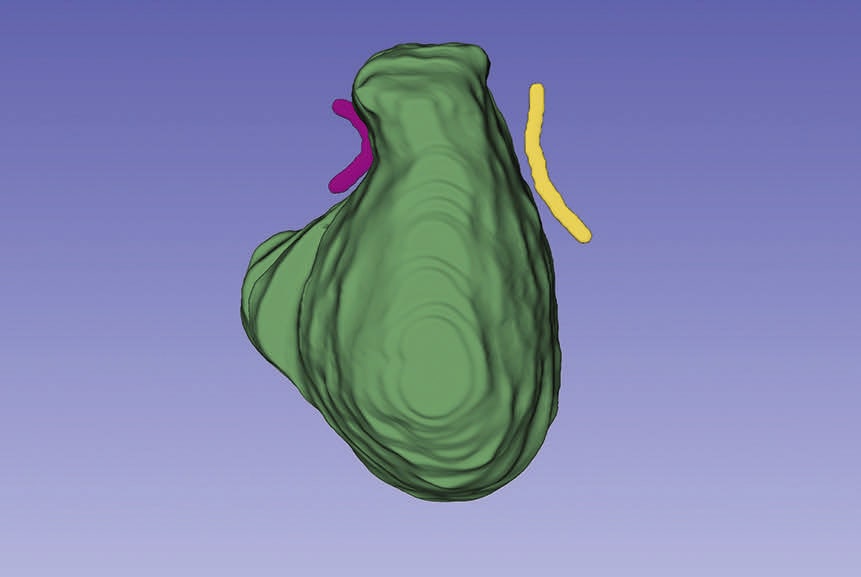
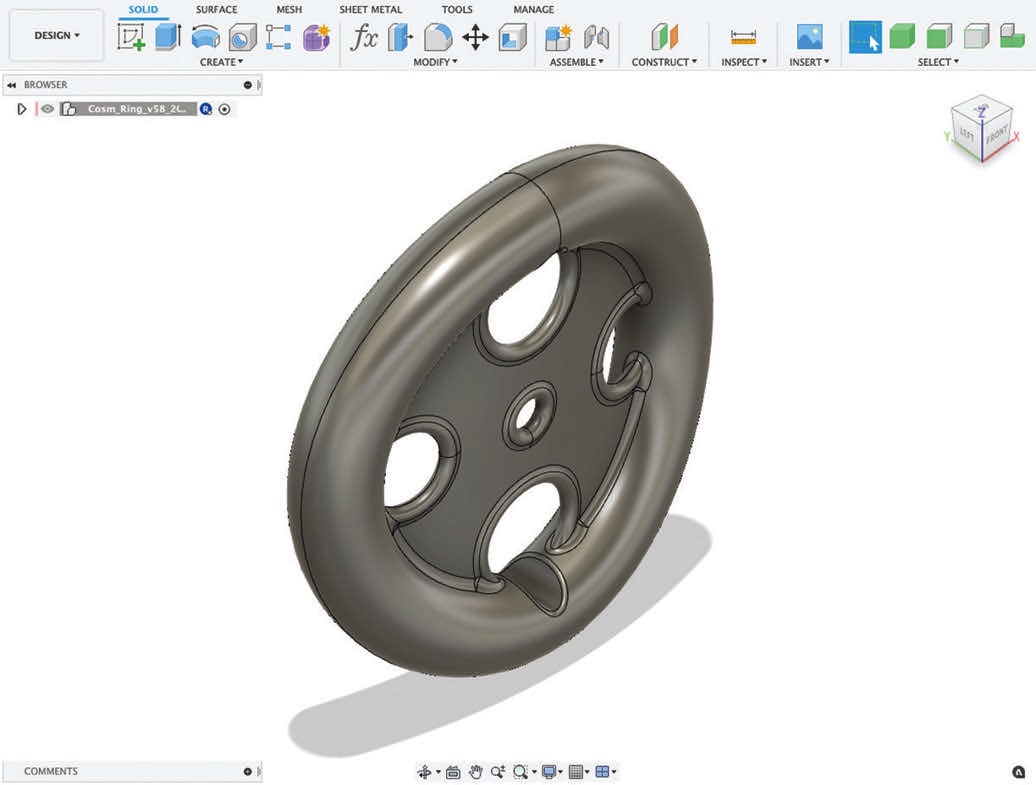
Cosm uses a new and proprietary ultrasound-based technique to scan and mold a patient’s pelvic floor and vaginal cavity. Advanced technologies such as machine learning and AI are used to analyze the ultrasound images and soft-tissue measurements, which help clinicians personalize pessaries for their patients. The measurements go into a parametric 3D model using Autodesk Fusion 360. Inputs can also include a patient’s treatment goals and activity level.
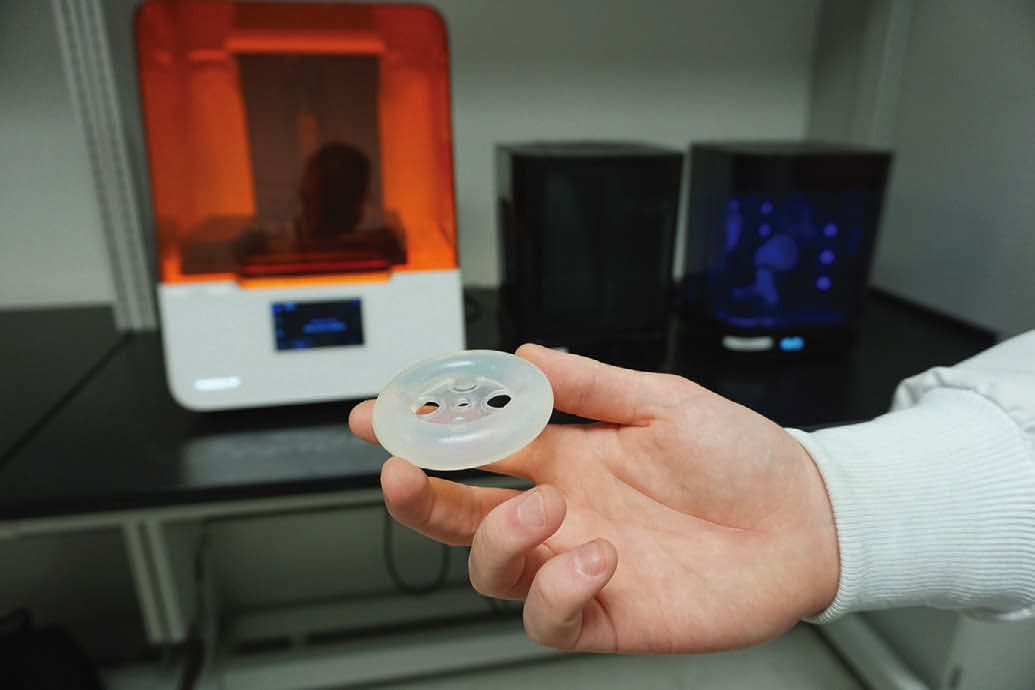
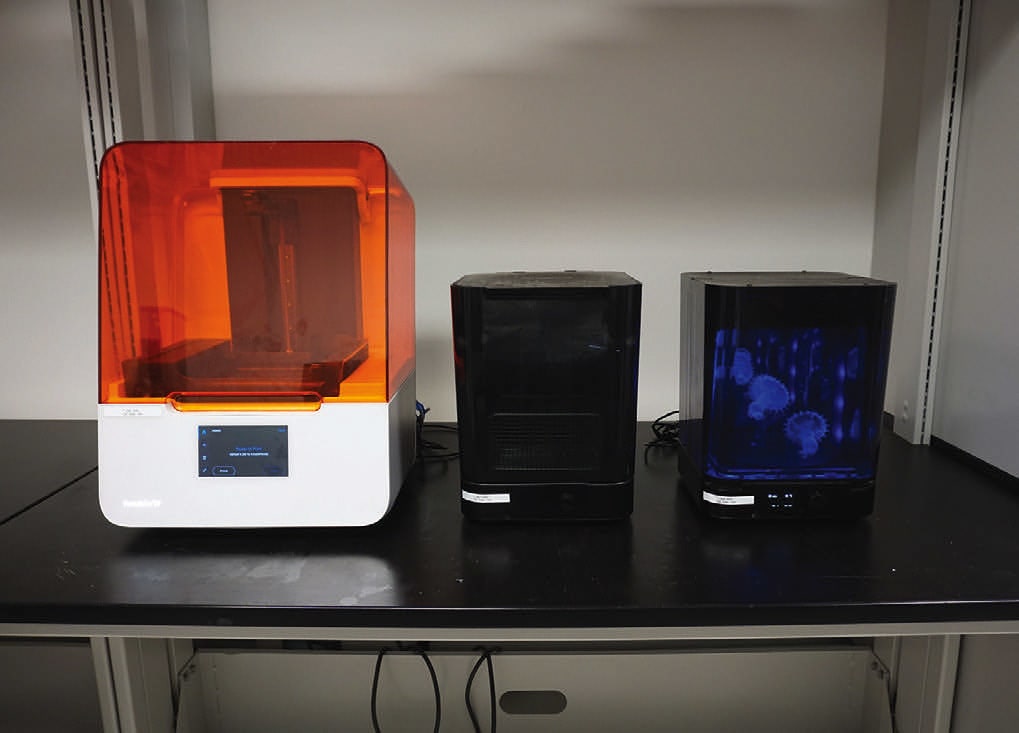
Cosm can achieve this mass customization and on-demand production through its use of Fusion 360 and Formlabs desktop 3D printers to produce high-fidelity silicone molds. “Fusion 360 is able to take in our sizing measurements and build a patient-specific model and mold for our device through parametric modeling,” says Robert Lancefield, mechanical design engineer at Cosm. “It can then export our molds to load into PreForm [software from Formlabs], which simplifies the process of uploading and tracking prints on the Form 3B. This entire process ensures the economic viability of our product in the long term by automating many steps in the custom-device creation process.”

The Formlabs Form 3B is a stereolithography printer designed to print with a suite of biocompatible resins, ideal for medical device workflows. The printers are capable of rapidly, accurately, and cleanly producing parts. The Form 3B offers excellent prints, a surface quality that requires minimal postprocessing, and a tight tolerance that minimizes the discrepancies from CAD to print. “That’s helpful for us since we want close tolerances and consistent product properties,” Lancefield says. “With the Form 3B’s resolution, we can vary our dimensions by a fraction of a millimeter in Fusion 360 to get the properties we need from our molds and final silicone parts.”
The Form 3B enabled Cosm Medical to continue development in the early stages without incurring the costs, setup, and space that industrial printers typically demand.
Tech Advances That Matter
At least two groups since the 1980s have attempted customized pessaries but failed. Sham says technological progress has made Cosm’s platform both technologically and economically viable — particularly the reduced cost and increased quality of ultrasound imaging, AI, CAD software such as Fusion 360, 3D printing, and cloud computing. “Ultrasound, for example, is extremely cheap relative to what it was just a few decades ago,” he says. “The $5,000 to $10,000 point-of-care ultrasound probes you can get now are arguably as good, if not better, than some of the $50,000 to $100,000 ultrasound machines just a few decades ago.
“We are excited by our growing momentum and milestones we’ve achieved so far on our path to serving clinicians and patients in need by modernizing the age-old pessary,” Sham continues. Cosm has been awarded two U.S. patents so far within its growing intellectual-property portfolio. In addition, Sham says Cosm has met with both the U.S. Food and Drug Administration and Health Canada and has a clear path for regulatory approvals in North America.
Cosm will deliver Gynethotics through a seamless digital platform for clinicians and patients, much like Invisalign in dentistry and some of the custom hearing products in audiology. The company plans to sell Gynethotics as a premium conservative therapy — much like how custom orthotics were introduced when only Dr. Scholl’s orthotics were available — and an alternative to existing treatment options. Standard pessaries cost between $50 and $150, but that money is wasted if patients can’t find the right fit and stop using them. Surgeries, Sham says, cost between $5,000 and $50,000 and have complication and reoperation risks.
Cosm’s work shines a light on a common, growing, under-served, and global women’s health issue. Whether it’s an individual’s struggle or a loved one’s, it’s clear that the old way of doing things is not sufficient, and this new solution could positively impact many lives.
References
- S. Shah, et al., “The history and evolution of pessaries for pelvic organ prolapse,” Int Urogynecol J Pelvic Floor Dysfunct, 2006 Feb; 17 (2):170-5.
- S. Sarma et al., “Long-term vaginal ring pessary use: discontinuation rates and adverse events,” BJOG, 2009 Dec; 116 (13):1715-21.
- I. Nygaard, et al., “Prevalence of Symptomatic Pelvic Floor Disorders in US Women,” JAMA, 2008 Sep 17; 300 (11): 1311– 1316.
This article was written by freelance writer Megan Nichols, with additional reporting by Paul Sohi, Product Marketing Manager for Autodesk. A version of this article originally appeared on Autodesk’s Redshift, a site dedicated to inspiring construction, manufacturing, engineering, and design leaders. For more information, visit here .