Semiconductor chip technology has miniaturized by leaps and bounds over the past couple of decades, enabling the modern era we live in with smartphones, tablets, and small electronic gadgets everywhere. However, battery technology, which provides the lifeblood to power these devices, has been at a near standstill since the commercial availability of lithium-ion batteries in the early 1990s. In no other application is this discrepancy more profound than in medical implants.

The battery is currently the largest component of the implantable medical device, making them bulky and thereby restricting applications inside the human body. Limited battery lifespan is also why implants generally need replacing, requiring otherwise unnecessary patient surgery while also bringing the risk and expense that comes with any surgery. Efforts are underway to produce the next generation of batteries that go beyond the capability of the lithium-ion battery. In the meantime, new innovations in ultra-low power electronic technology have arisen as the greater potential than battery chemistry to revolutionize medical implants. The significance of recent developments in the areas of wireless charging and energy harvesting to power implanted medical devices is worthy of discussion.
Wireless Charging
The concept of wireless charging—where the battery of a device is recharged using wireless electricity—is catching on for consumer electronics. The Wireless Power Consortium estimates that 50 million chargers were sold in 2014, and top-of-the-line phones are starting to come with built-in wireless charging capability. Wireless charging through the human body to power implanted devices has presented a challenge until now.
In 2014, Stanford University reported that researchers have found a way to extend the wireless charging capability that is available now for devices from cell phones to implantable devices. The discovery allows a power source about the size of a credit card to be held over the body to wirelessly transfer power to an implanted medical device as small as a grain of rice. The implications are astounding. Not only can pacemakers, for example, be miniaturized down from the size of a quarter and last the lifetime of the patient, but the technology also opens the doors for new medical implant applications such as deep brain and body tissue stimulation. The ability for doctors to treat diseases and illnesses with electronic therapy embedded in the body instead of prescribing drugs is a profound alternative. The electrical treatment may be even more effective since specific circuits of the brain can be targeted for example, while drugs affect the brain more globally.
The key to this advancement is in the strength of the electromagnetic field. In wireless power technology, electricity is induced in inductively coupled coils in the receiving device (the implant) using electromagnetic waves from a power source. In cell phones and other small device wireless charging applications, such as rechargeable toothbrushes, these waves are in the near-field frequency spectrum.
Near-field waves decay quickly and cannot reach small medical devices deep inside a body without requiring large receiving coils, though they are useful in less deeply embedded devices such as hearing implants. Far-field waves, such as radio communications, can travel over longer distances, but are not suitable for biological tissue applications as they either reflect off the body or are absorbed as heat. The Stanford inventors were able to develop an “in-between” technology that they call midfield wireless transfer, which can safely penetrate the body without interacting with biological tissue. (See Figure 1)
To demonstrate the mid-field wireless charging technology, the Stanford researchers built a pacemaker the size of a grain of rice. Complete with a microchip and power harvesting coils, the pacemaker can be situated anywhere inside the body and does not require a battery. A battery could be added however, to provide power storage for higher power applications.
The mid-field charging technology still needs to be tested in humans and receive safety and efficacy approval, so it could be several years before its adoption in commercial medical devices.
Energy Harvesting
Today’s miniaturized circuits can do more in less area, all while consuming less power. Ultra-low power electronic implantable medical devices are able to operate battery-free on the small amounts of power that can be gleaned from ambient sources from the human body such as body motion or heat, while larger implanted devices can use harvested energy to supplement the battery and reduce its size. In fact, energy harvesting has proven to be an effective alternative to pure battery power in medical implant applications given the ability to produce power from nanowatts to several milliwatts, which is in the power consumption range of the most common implantable medical devices today.
Different types of energy can be harvested from a variety of sources. For example, solar energy can be collected from the environment. Kinetic energy can be derived from the motion of human activities, such as running or walking. The body can provide thermal energy. The challenge that designers face in implantable medical device applications is the need for a constant and perpetual energy source.

Fortunately, the human body has the remarkable capacity to regulate to a fairly constant core temperature even as the ambient temperature changes. Thermoelectric harvesting technologies take advantage of human body heat, and are now able to produce a few hundred microwatts. This amount of power is suitable for minimal power applications such as implanted nerve and muscle stimulators or cochlear hearing implants.
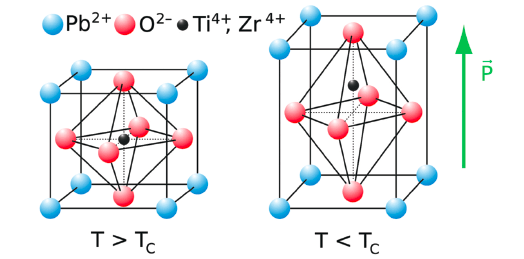
Piezoelectric materials provide another promising approach to energy harvesting for implanted devices, as reported by mechanical engineers at the University of Buffalo in IEEE Spectrum. These materials respond with an electrical polarization that is proportional to an applied mechanical strain, and are thus used to convert mechanical motion to electrical energy. The movements of a beating heart are apparently sufficient. Earlier this year, and published in the Proceedings of the National Academy of Sciences of the United States of America, researchers at the University of Illinois at Urbana-Champaign reported on a new harvesting device that can be surgically applied onto the heart to generate power from the moving organ. The flexible device, roughly the size of a postage stamp, incorporates a piezoelectric material called lead zirconate titanate onto an ultrathin compound. The energy produced when the device flexes with each pulse is stored in a miniaturized battery, and is enough to power a pacemaker. (See Figures 2 and 3)
Other energy harvesting options include electrostatic transduction, magnetic induction, and blood sugar oxidation. With the great potential that energy harvesting brings to consumer electronics and wearable technology as well as the medical market, many exciting developments in these and other harvesting techniques are guaranteed.
Summary
As the world waits for the next generation of batteries, wireless charging and energy harvesting are the low power technologies that are propelling the implantable medical device industry forward. Releasing the designs of future medical implants from the size and lifespan constraints caused by the battery, new product innovations in these areas will transform the medical industry for years to come.
This article was written by Landa Culbertson, Technical Writer, Mouser Electronics, Mansfield, TX. For more information, Click Here .



