Doctors often tell patients to “listen to your body and take note of what it is telling you.” Now, technology is being developed that will listen for us and process the signals to help identify the best course of action.

The trend toward an aging population is well reported, as is the sustained reduction in global birth rate. Together these forces mean there will be fewer people able to care for a larger elderly population in the coming decades. Nothing can be done in the short term to change these social statistics, but technology, it seems, may be able to step in and lend a helping hand both figuratively and perhaps even literally.
As integrated semiconductors continue to shrink in size but expand in capabilities, the concepts of artificial intelligence (AI), cloud computing, and ubiquitous connectivity are coming together in a disruptive way that will change the healthcare industry for good and the better. The possibilities are vast, demand is growing, and the will to make a positive difference is inherently humane.
Today, wearable technology is epitomized by small devices most commonly worn on the wrist that monitor activity and the wearer's statistics such as pulse rate; in short, it is an augmentation that is consciously affected. As technology develops, the technology of tomorrow may well be woven directly into the fabrics we wear, making it less intrusive and therefore much more easily assumed.
Smart fabrics, as they are commonly called, have the potential to change the way we monitor many things, but perhaps their greatest potential lies in healthcare. Using technology to monitor a patient's condition and apply medication is an incredibly active area of research, with results already appearing.
Feeling the Pressure
During recuperation, the pressure exerted by or upon an area of the body can be a particular cause for concern. Swelling is part of the healing process, but it must be monitored, as it can also be a precursor to secondary infections, for example. Similarly, if a patient doesn't move regularly, he or she can quickly develop pressure sores that can inhibit the healing process. The answer is to monitor the patient's wounds and their general movement, or lack of it.
One way of achieving this is to use sensors that can be woven into bed sheets or clothing; silicone-coated, electrically conductive yarn, woven into bedding, is in development. It allows moisture and movement to be monitored and alerts care providers when a patient needs attention. The same technology is being used to enable hospital beds to automatically move in accordance with the patient's needs, thereby reducing the burden on care providers.

The same principles are also being integrated into dressings and bandages to monitor the pressure exerted by the body as it heals, indicating whether the dressing is too tight, for example, or to record how quickly swelling in the affected area reduces.
There are many ways to measure the pressure of any given medium; historically, blood pressure is recorded by measuring how much pressure is required to stem the blood's flow. This process can now be automated using pressure sensors mounted in-line with the compressed air used to exert the pressure. As a result, blood pressure monitors have become consumer devices that can be used by anyone, in the comfort of their own homes. It isn't a huge leap to integrate the same technology into fabrics such as sports clothing.
Pressure sensors are also being used in other ways, such as in shoe insoles, where they are used to monitor the gait and activity of a patient who may be suffering from peripheral neuropathy; a condition that stops the brain from receiving information from an area of the body, such as the foot. Figure 1 shows such a system from Orpyx that records data from an insole and transmits it wirelessly to a smartphone application. By using sensors to monitor the pressure on the foot and provide the feedback to the patient, it can help prevent ulcers forming, which, in extreme cases, can result in the need for limb amputation.
Embedding sensors into a dressing enables the pressure exerted by a swollen limb to be assessed by measuring the distortion of the skin; this is the kind of 'smart fabric’ now being developed by researchers.
By integrating pressure monitoring directly into smart fabrics, long-term trends can be identified more easily, helping facilitate early diagnosis of conditions such as cardiovascular disease, for example.
A Smarter Plaster
Measuring hydration levels through monitoring changes in the electrical characteristics of skin is now becoming a reality thanks to developments in nanotechnology. By embedding tiny wires into stretchable fabrics applied directly to the skin, small electrodes can monitor hydration and communicate that in real-time. The same technology could be applied to clothing.
A similar and effective method of diagnosis being employed in smart dressings involves passing a small electrical current through the body's cells and measuring their impedance, a significant extension to a technique called impedance spectroscopy. Measuring the changes in capacitance and resistance presented by cells as they decay can be used to create smart bandages that can identify bedsores before they become visible to the human eye.
While electronics are a significant part of the smart fabric solution, developments in traditional forms of healthcare, which includes looking at how medicines can be applied more effectively, are also part of the solution. The potential to empower a smart dressing to not only monitor a wound but also directly apply medicine has been demonstrated by a team of researchers from the University of Nebraska-Lincoln, Harvard Medical School, and MIT.
The researchers have created the first bandage capable of dose-dependent drug releases, such as pain killers and antibiotics, as well as medication to promote faster healing and tissue regeneration. In essence, it works by implanting the medicines inside a gel, which, in turn, coats wires that are woven into the bandage. A microcontroller, also embedded into the bandage, controls a current flowing through the wires, causing them to heat the gel and release its payload directly to the affected area. Trials have shown positive results, and the team is now working on integrating sensors to measure indicators such as glucose and pH levels to fully automate the drug-delivery process.
Connected Medicine
Throughout the Internet of Things or IoT, wireless connectivity provides a way to push data up to the cloud, where AI can be used to identify trends in a big data way. By applying this process to the Internet of Medical Things (IoMT), that data could ultimately be used to improve the way other patients with similar conditions are treated.
This will require a more holistic approach to using technology in the medical sector, bringing together multiple disciplines into a single solution.
Researchers at the Institute of Life Science, part of Swansea University, are looking into how sensors enabled by the latest developments in nanotechnology can be integrated into smart bandages that also include 5G connectivity to not only monitor wounds but also to communicate that information to caregivers, remotely, in real time. The approach would also employ 3D printers to manufacture the bandages.
Nanotechnology is closing the gap between the biological and technological worlds and will be an enabling technology for the IoMT; research into how nanoparticles can deliver treatments to specific cells in a body is well under way and already showing some positive results. One of the initial benefits of targeted treatments at the cellular level is that the body no longer needs to metabolize a drug for it to be distributed around the body, which will result in lower dose levels, more effective treatments, and ultimately lower costs for health providers.
MEMS in Medicine
Microelectromechanical systems, or MEMS, technology has already helped shape the mobile phone sector by providing accurate three-, six-, and nine-axis motion sensing in tiny packages. The same technology is used extensively in wearable fitness trackers. MEMS microphones have revolutionized hearing aids, but their potential goes much further.

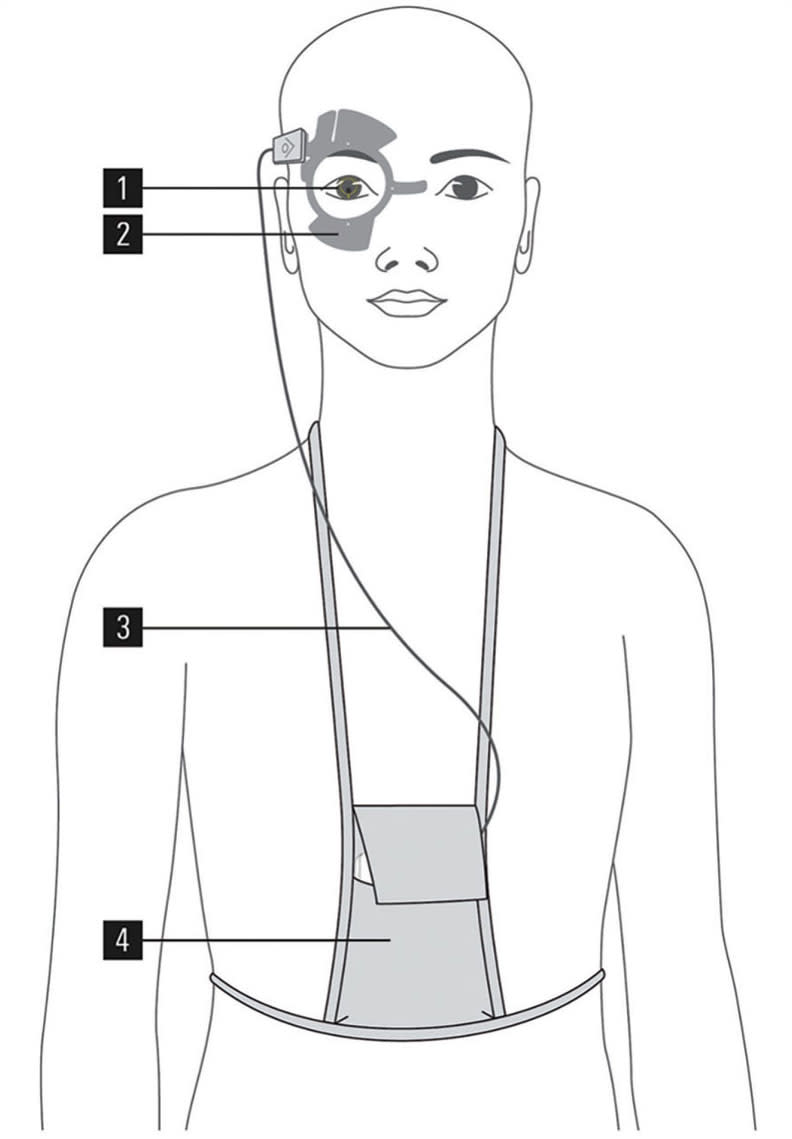
By mounting a MEMS microphone directly onto a disposable contact lens, it is possible to measure changes in the intraocular pressure (IOP) of the eye, which indicates changes in the shape of the cornea, an early sign of glaucoma. MEMS-enabled IOP sensors that include wireless communication are now available from the Swiss company, Sensimed. Figure 2 shows how the system comprises three elements: the disposable contact lens with an embedded sensor and transducer, a separate antenna that is worn around the eye, and the data recorder, all connected by a thin wire.
The system uses near-field communication (NFC) technology to wirelessly power the sensor, which is enough to make the measurements and transmit that information back to the antenna. This approach has the potential to be used in a wide range of IoMT devices because it removes the need for a hardwired power source (typically a battery), which can easily be the largest part of the system. By exploiting the features of NFC, many other types of sensors could be embedded within smart fabrics alongside the microelectronics needed to control them.
Conclusion
Smart fabrics are changing the nature of healthcare and are enabled by the unprecedented cross-fertilization of technologies. While many still only exist in research laboratories, the pace of development is increasing, and the IoMT holds the potential to change the doctor-patient relationship forever.
This article was written by Rudy Ramos, Project Manager for the technical content marketing team at Mouser Electronics, Mansfield, TX. For more information, visit here .



