In neurology, a quiet crisis has emerged: the supply of specialists can no longer meet the rising demand for diagnostic interpretation.
By the end of 2025, sources have already predicted that the demand for neurologists will exceed the supply by 19 percent. Furthermore, rural areas already have 80.5 percent less access to neurologists compared to metro areas. 1
This shortage has created not only staffing strain but also a data bottleneck. Nowhere is this more evident than in EEG interpretation: a domain where AI-assisted systems are beginning to make a measurable impact.
These recordings are essential for diagnosing epilepsy, seizures, and brain injuries, yet many hospitals face review delays of 24–48 hours or more. In acute neurological cases, that delay can alter outcomes.
So, how do AI-assisted programs fit into the EEG picture? That’s what this article will explore.
EEG Data Volume Has Outpaced Human Capacity
Advances in EEG technology have multiplied the volume and duration of recordings. A single long-term or ambulatory EEG can span days, producing tens of thousands of signal segments that each require expert review.
Unlike imaging, EEG signals have inherently low signal-to-noise ratios and high variability between patients. Artifacts from movement, muscle tension, or external interference complicate interpretation, and context such as medication, sleep state, or concurrent conditions adds layers of nuance.
The truth is that manual review is no longer scalable. The backlog now seen in many hospitals represents a design bottleneck as much as a clinical one. Engineers face the task of developing systems that can process vast, noisy datasets accurately and quickly, all without disrupting established clinical workflows or eroding physician trust.
The Engineering Constraints of Scalable EEG Review
To make AI clinically viable in neurodiagnostics, several engineering constraints must align. From latency and accuracy to clinician trust, data security, and infrastructure, each design decision affects performance, usability, and regulatory compliance.
Latency and Accuracy. EEG interpretation is a time-sensitive task. AI systems must flag abnormal activity in near real time so that clinicians can intervene when it matters most.
At the same time, accuracy must balance sensitivity and specificity, minimizing both missed events and false alarms that could erode confidence or delay treatment.
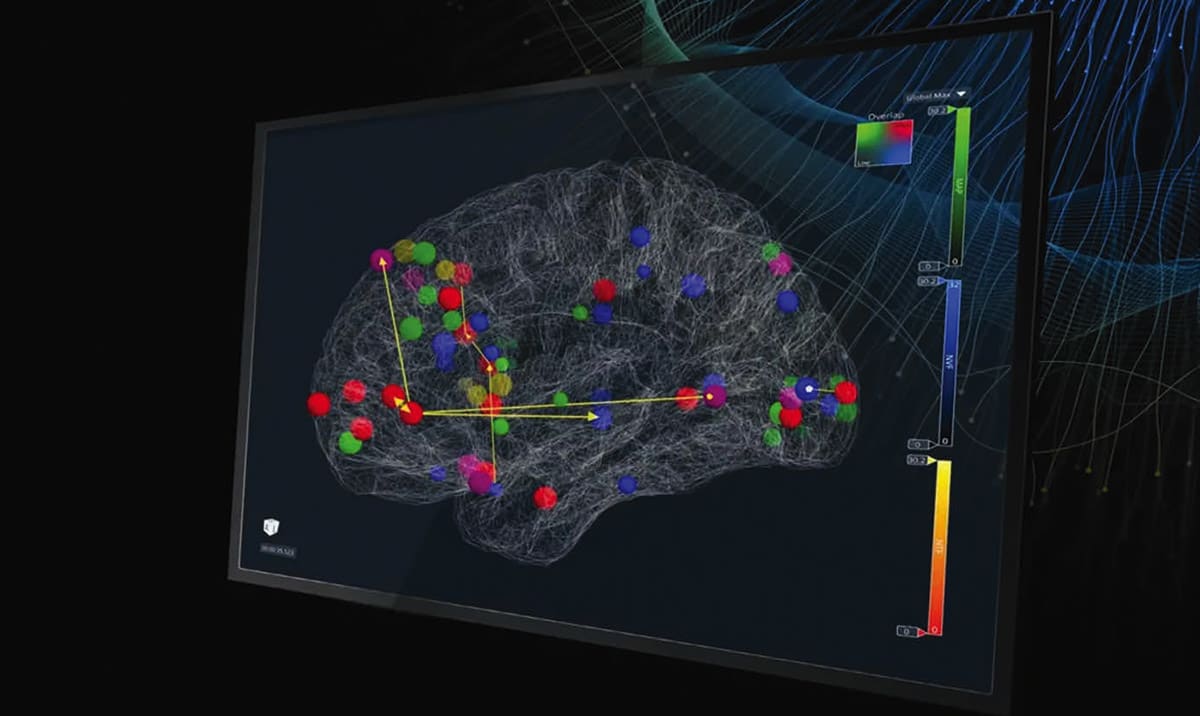
Clinician Trust and Explainability. No matter how advanced the algorithm, a system without transparency will fail in clinical use. Neurologists must see what the model detected, why it was flagged, and how confident the system is. Explainable design, intuitive visualization, and audit trails build the trust needed for consistent adoption.
Data Security and Regulatory Compliance. EEG recordings contain sensitive patient information, so every stage of the workflow must meet strict security and privacy standards. Systems need to integrate safely with existing hospital IT environments, comply with HIPAA, and maintain full traceability.
Because this is a regulated medical domain, validation and continuous postmarket monitoring are non-negotiable.
Infrastructure and Deployment. Hospitals often operate on legacy networks and limited on-premise computing power. Engineers must decide whether to process EEG data locally or leverage cloud scalability for faster throughput and collaboration.
Striking the right balance between speed, control, and cost remains one of the most practical design challenges in bringing AI-based EEG systems to scale.
The Technological Solution: Inside the NeuroMatch Platform
LVIS Corporation approached this challenge through NeuroMatch®: an AI-enabled platform that accelerates EEG review without removing clinicians from the loop. The system applies deep-learning models trained on thousands of hours of multi-channel EEG data to identify seizure activity, spikes, and other anomalies across complex signal patterns.
A critical component of the design is artifact reduction. By filtering out non-neurological noise (such as eye blinks or muscle movement), the system reduces false detections and allows neurologists to focus on the signal segments most likely to hold diagnostic value.
Once processed, NeuroMatch presents results through a secure browser-based interface. Clinicians can view annotated EEG traces, confirm or override flagged events, and generate reports directly from the dashboard.
Because the system integrates with standard EEG file formats and existing hospital hardware, it fits within current workflows rather than replacing them.
NeuroMatch operates primarily as a cloud platform, enabling rapid processing and collaboration across facilities. The design preserves what LVIS calls a “human-in-the-loop” model: the AI triages, but the neurologist decides.
Validation and Usability: Building Confidence Through Testing
Performance validation was a cornerstone of NeuroMatch’s development. Engineers benchmarked the system’s seizure- and spike-detection accuracy across large, annotated datasets, measuring sensitivity, specificity, and end-to-end processing time.
Security and compliance were addressed through role-based access control, encrypted transmission, and HIPAA-aligned data management. In real-world deployments, NeuroMatch has already demonstrated measurable impact, compressing EEG review times from days to hours in hospitals across the United States and South Korea.
The Broader Impact: Expanding Neurological Capacity
AI-assisted EEG systems like NeuroMatch represent a shift from automation to augmentation. Instead of replacing clinical expertise, they multiply its reach, allowing each neurologist to handle more studies, more efficiently, with greater consistency.
This acceleration in data review directly affects patient care. Faster triage of abnormal EEG segments can shorten the time to seizure diagnosis, expedite medication adjustments, and improve monitoring for postoperative or ICU patients.
For regions already struggling with limited neurology access, that improvement in turnaround time can translate to earlier intervention and better outcomes.
The approach also sets a precedent for scalability in other data-heavy medical domains. As wearable neurosensors, continuous monitoring systems, and home-based EEGs become more common, the ability to process and prioritize long-duration signals will define the next generation of digital neurodiagnostics.
A New Model for Neurology’s Capacity Crisis
The neurologist shortage is already a present constraint. EEG data volumes have surpassed what human reviewers can manage, creating a genuine bottleneck in neurological diagnostics.
By addressing this as an engineering problem rather than a staffing one, LVIS Corporation has shown how thoughtful design can expand capacity without sacrificing oversight.
Through deep-learning signal analysis, and clinician-centered workflows, NeuroMatch turns the EEG backlog into a manageable, data-driven process. In doing so, it illustrates a broader truth about medical innovation: when technology is designed for transparency, speed, and collaboration, it empowers clinicians to care for more patients, faster, and with greater accuracy.
This article was provided by LVIS Corp., Palo Alto, CA. For more information, visit here .
References
- Jeremy Alexander, “3 Stats About the Neurology Shortage that Should Get Your Attention,” Locumens.com.



