Heading into 2020, the medical device industry enjoyed promising market conditions. KPMG released a study in 2019 that showed annual sales of medical devices were expected to climb an average of 5 percent annually for the next decade, with 2030 culminating in a $800 billion global market. The U.S. market was the largest component of those escalating revenue figures, with an expected 2030 volume of $180 billion. Much of that growth was expected to be driven by new technologies — surgical robots, 3D printing, telehealth, predictive analytics, and other emerging solutions have all gained the attention of every forward-thinking health system and hospital in the world.
By early spring of 2020, however, the promise of 5 percent annual growth was replaced by a large crater in revenue numbers caused by the global coronavirus pandemic. Medical device manufacturers — except perhaps some of those producing ventilators or patient monitoring technologies — experienced weekly, monthly, and quarterly revenue shortfalls of 60 percent or more. Sales of anything outside of the COVID-19 world generally stalled. Trials of new technologies were halted. Budgets were frozen. And salespeople weren’t permitted inside hospitals. Very few of the 7,000+ hospitals in the United States were scheduling or performing elective surgeries — or even thinking about the acquisition and deployment of new technologies.
While the number of coronavirus cases in the United States hadn’t tapered off by the middle of summer, many Asian and EU countries began reporting lower infection numbers. Hospitals in those countries began performing elective surgeries, restarted technology trials and began to recoup some of the revenue lost during the COVID-19 crisis. Even in the United States, where cases were still increasing in most states, health systems and hospitals restarted elective procedures in the OR and started ramping up again. This small global uptick in hospital revenue has been accompanied by encouraging news on the coronavirus vaccine and treatment fronts, as several companies announced success in phase II and III trials.
This news points to a slow but steady global recovery that will likely allow medical device manufacturers to recoup some lost revenue and restart trials. But even as the recovery inches forward and hospitals begin to recover themselves, the market going forward will be changed. Capital conservation will likely be an agenda item for every health system and hospital CEO for the next couple of years. This means supply chain teams will likely be getting a seat in more and more C-level meetings. Health systems and hospitals, especially in the United States and other for-profit markets, know they need to innovate and demonstrate progress in order to attract patients and build loyalty in a new consumer-driven climate. This could give rise to new buying processes that include evaluating the clinical efficacy, impact on revenue generation, and return on investment of medical devices.
In other words, the promising medical device market projected in 2019 will, in all likelihood, return — but it will look and operate much differently than it did in the pre-pandemic days. This will almost certainly lead to changes in innovation and engineering processes in medical device companies. There had already been a move on the part of many manufacturers to engage suppliers with strong engineering teams in collaborative development models before the pandemic. Now, as healthcare emerges in a permanently changed state, the need for new ideas that improve clinical outcomes while still conserving capital will be in demand.
Rationale for the Rise in Collaborative Engineering Initiatives
While no recent formal study quantifies the reason for an increase in engineer-to-engineer (E2E) efforts between manufacturers and their vendors, there has been some anecdotal evidence. Medical device manufacturers have found that there are three reasons for collaborative design efforts — speed to market, risk mitigation, and cost reduction.
While medical device manufacturers typically have strong connections with their customers and ample engineering talent within their businesses, companies that are smaller and more agile tend to offer research, development, and design processes that allow products to move through various engineering phases quicker and, ultimately, get to market faster.
The typical horizon for medical device design and manufacture tends to be in the three- to five-year range. This timeline can work in a normal market, but given the pause most companies took in terms of revenue generation due to the pandemic, it’s not likely to deliver desired financial results. And while some devices go through the research, design, development, and manufacture process in a one- to three-year window, it’s less common. In most of those cases, these condensed schedules only exist when an external team of engineers collaborate closely with manufacturer’s engineering team to intentionally expedite the timeline.
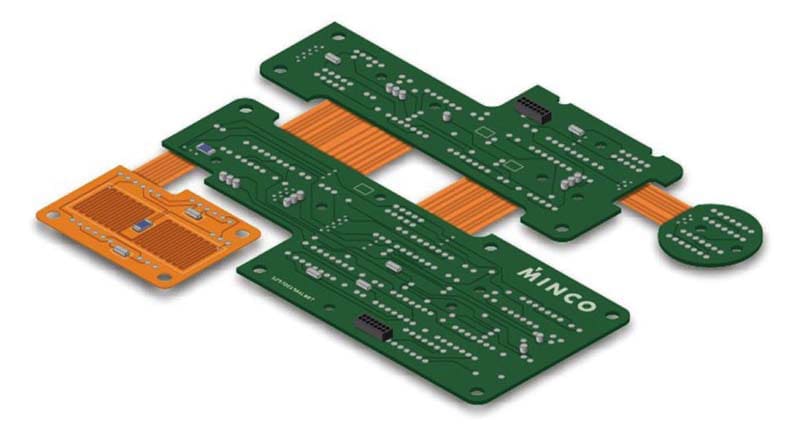
Innovation is another driver for collaborative or E2E initiatives. The sheer size of most medical device organizations tends to slow the research and development process. It’s simply a challenge to get larger organizations to move with the agility of smaller companies. Medical device companies tend to have strong ideation capabilities, are close to the customers so they know what the market wants, and they’re good at anticipating emerging needs. But the best collaborative experiences typically have one thing in common: a clear idea of what they want to achieve as an end-product — then the team works with the manufacturer’s engineers to develop circuits-sensor-and-heater packages that bring that vision to life. Bringing an experienced engineering team into the process early tends to deliver the best result from an innovation perspective. The risks of delays — in both the engineering and manufacturing process — are greatly diminished by following this kind of collaborative process.
Integrating engineering teams in a collaborative process also tends to deliver measurable cost reductions — both in design and manufacturing. This requires engineering leaders with the experience to know that the real cost of bringing a product to market involves the entire life cycle — design, manufacturing, and performance in the field. Engaging vendors in the earliest design phases tends to eliminate false starts, rework, complications on the production line and, in some cases, problems related to recalls or product returns once products are in the field.
Five Simple Tips for Getting the Most from an E2E Engagement
Engineers love challenges. Or as Thomas Edison said, engineers always seem to know there’s a better way to accomplish the task at hand — it’s just a matter of finding it. Creating something new and better typically requires integrating flexible circuits, heaters, and sensors into a single package that saves space, cuts costs, or improves performance. Here are five tips for getting there as efficiently as possible:
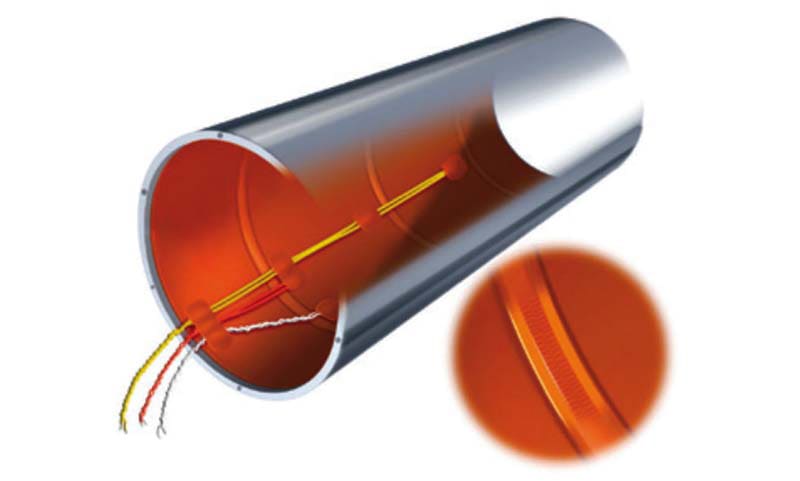
- Start Simple. In many cases, customers begin by asking their partner to design something specific, like a flex circuit. Through collaboration, the team discovers that integrating a heater and/or a sensor can create a package that’s lighter, more resilient, and more efficient on the production line. For instance, an environment may need to remain thermally stable, so flex engineers collaborate with thermal solution engineers to design a product that exceeds the initial customer requirements.
- Collaborate Early. Most performance improvements, space reductions, cost savings, and new capabilities that integration can achieve are discovered and tested early in the design process. Engaging flex circuit, heater, and sensing experts from the beginning of a project keeps the focus on larger program objectives and provides more runway for new ideas.
- Seek Deep Expertise. Experienced engineers can take an OEM’s flex circuit requirements, apply thermal modeling techniques, and integrate a heater to meet specific needs. E2E discussions can lead to material selection and heater designs that meet specific watt density requirements while still providing high yields. This helps control cost and makes for more predictable delivery schedules.
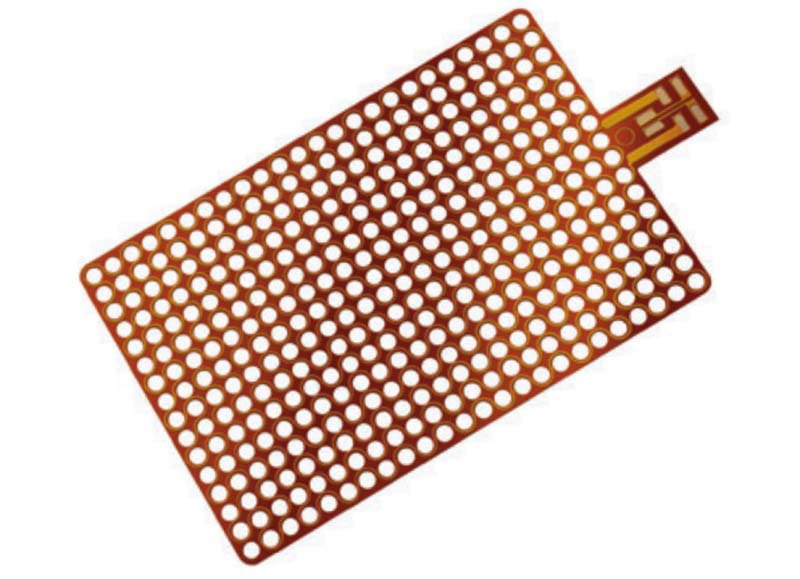
- Think Integration. Using some of the same substrates as flexible circuitry enables integration of a flexible heater. Newer designs often include adding layers that offer lower resistance — and carry power and data signals to other portions of a device. Be sure to seek out engineers who are IPC-certified and proficient in IPC 2223 (design standard for flexible circuits). They’ll be better positioned to help navigate critical considerations, including material stability, the ability to plate on multiple conductive surfaces, how to drill accurately and cleanly, and the bonding of these various materials.
- Add Sensing to Packages. This can be done through a variety of surface mount off-the-shelf sensors. Both flexible circuits and flexible heaters lend themselves to pick-and-place technology. Be sure to choose engineering teams that are fully up to speed on IPC 610 as well as J-STD specifications for soldering.
Case Study: Achieving Differentiation through True Innovation
A medical device company was looking to create strong differentiation with surgeons and hospitals who are flooded with new product ideas almost every day. The integration challenge was considerable: the customer’s engineers wanted to develop a device capable of cauterizing exit wounds in femoral arteries. Wounds caused by the removal of catheters during heart procedures were taking hours to heal with existing technology. This presented serious risk for patients and tremendous liability for both surgeons and hospitals. Engineers working for the medical device manufacturer believed they could close the cauterizing gap to six minutes — instead of hours — but they needed a compact and reliable integration of a flex circuit, heater, and sensor.
Minco was challenged to integrate a flex circuit with a heater and sensor to create a highly reliable device that was able to reach a target temperature of 100 °C in less than six minutes — then hold that precise temperature while the wound cauterized. Presenting additional challenges, the finished component could be only slightly larger than a catheter — a donut shape with a 4 mm (0.16 in.) outer diameter and 1.5 mm (0.06 in.) inner diameter. Minco designed a flex circuit integrated with an all-polyimide heater, which was created using a special adhesive-free process that allowed for higher temperatures than conventional offerings. The circuit itself was not only complex in its size — limited real estate meant the elements had to be stacked on top of each other — but there were also 22 blind micro vias (0.08 mm) for power as well as two 0.15 mm blind vias to carry the signal of the surface-mount NTC thermistor that sensed the temperature of the heat sink.
Engineers from Minco and the manufacturer were able to take the product design to a new level and achieve the cauterizing goal by integrating flex circuits, heaters, and sensors into a single device. This new configuration achieved the challenging temperature goals, saved space, and improved reliability in the field by reducing the number of failure points.
This article was written by Chris Clark, Product Manager at Minco, Minneapolis, MN. For more information, click here .