Traditionally, toxicologists and biocompatibility experts considered the materials in breathing gas pathways as external communicating devices and evaluated these materials according to the ISO 10993 series of international standards. 1 In the past, testing laboratories would refer to the ISO 109931 matrix of biocompatibility endpoints and simply check off the tests recommended for external communicating devices. Unfortunately, this approach leads to testing that provides questionable benefit and potential hazards being missed. In order to bridge these gaps in ISO 10993, ISO Technical Committee 121 released a new set of standards specifically geared toward the biocompatibility evaluation of breathing gas pathways in healthcare applications. 2 In March 2017, the committee published ISO 18562, a four-part standard aimed at providing the general framework required to adequately determine the acceptability of medical devices that contain breathing gas pathways. 2 This article takes a dive into the testing requirements of ISO 18562 and discusses the details necessary for medtech companies to satisfy this new standard.

ISO 18562 is comprised of four parts:
Evaluation and testing within a risk management process, 2
Tests for emissions of particulate matter, 3
Tests for emissions of volatile organic compounds (VOCs), 4 and
Tests for leachables in condensate. 5
Each of these sections is designed to address a potential hazard that is specifically associated with the breathing gas pathway of a medical device. The scope of devices covered by ISO 18562 can range from simple breathing tubes to complex gas mixing stations and ventilators. 2 Further, it includes any and all accessories of these devices that may come in contact with the gas stream before it reaches the patient. This does not only include devices that deliver air or oxygen to patients, but also those that deliver inert gases to patients, including nitric oxide and anesthesia. 2 The immense range of devices that may contain these potential hazards highlights the necessity for a specific set of standards dedicated to the evaluation of these breathing gas pathways.

In recent years, FDA has developed a renewed focus on limiting unnecessary testing with the biological evaluation of medical devices. Therefore, Part 1 of ISO 18562 follows very closely the general guidance for ISO 10993 in which testing and evaluation of these breathing gas pathways should fall under a larger risk management approach. 6 The first step in the evaluation and testing of breathing gas pathways of medical devices is identification of all the potential hazards to patients that are specifically associated with the gas stream coming from your device. These are the hazards that will be evaluated according to ISO 18562. However, this standard is not prescriptive when it comes to evaluating these hazards. It does include some specific details that need to be considered when designing a test plan. For example, ISO 18562 provides guidelines for parameters such as using the correct clinically relevant flow rates depending on the target patient population, sampling at adequate intervals throughout the testing depending on the duration of use of the device, and maintaining the correct temperature of the device during testing. 4 However, when it comes to the methods used to sample and measure the potential hazards associated with the gas stream, ISO 18562 only provides general strategies.
Hazards and Test Methods
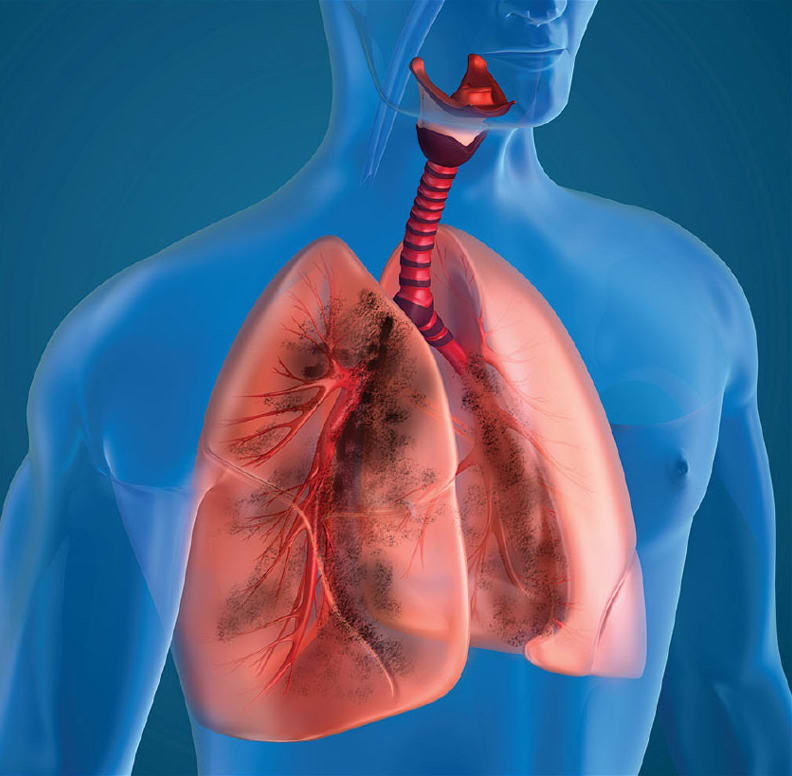
There are three main hazards that can be associated with the breathing gas pathways of medical devices. The first of these hazards are evaluated under Part 2 of ISO 18562, Tests for emissions of particulate matter. 3 There are two size ranges of particulates that needs to be measured, PM2.5 and PM10. PM2.5 includes all particles between 0.2 and 2.5 μm in size, while PM10 includes all particles between 2.5 and 10 μm.3 PM2.5 particles pose a more dangerous hazard to patients because they can bypass the human body’s natural defense mechanisms. This allows them to penetrate deeper into the patient’s lungs, causing significant health risks. ISO 18562-2 requires that the total mass of PM2.5 particles emitted not exceed 12 μg/m3 of gas. 3 PM10 particles pose fewer hazards but can still be dangerous to patients. These particles cannot penetrate as deep into the lungs. However, they still pose significant health risks to patients. ISO 18562-2 requires that the total mass of PM10 particles emitted not exceed 150 μg/m3 of gas. 3
Particulate Matter. ISO 18562-2 details two methods for measuring particulate matter emitted from medical devices. The first is a filter collection method that has been used for environmental testing for decades. 3 Conceptually, this is the simplest method that involves measuring the difference in mass of a filter before and after collection of particulate matter. Unfortunately, measuring particulate matter emitted from medical devices is not that simple. In most cases, the amount of particulate matter emitted from a medical device is minuscule. Therefore, one must pass sufficient gas through the filter to measure the change in mass. This can sometimes require an extremely sensitive balance and can be disrupted by the slightest artifact. Some recommend maintaining the filters in an environmentally controlled chamber for up to three weeks before and after testing to ensure that moisture accumulation does not impact the measurements. 7 In short, this method is not good for short duration tests where the amount of particulate matter will be diminutive.
The second method detailed in ISO 18562-2 for measurement of particulate matter emissions is a particle counter method. 3 This method uses an analytical particle counter or particle sizer to measure and count each particle emitted from the medical device. Particle analyzers employ a light scattering technique in which the gas stream from the medical device enters an isokinetic sampling probe and is directed past a laser that illuminates the particles. The light from the laser is redirected or absorbed and detected by the analyzer, allowing for accurate measurements of particulates. 7
As mentioned above, ISO 18562-2 specifies limits for particulate matter in total mass of particulates in the gas stream. Many particle counters and sizers will output a total mass of the measured particulates. However, for those that only provide a count of the number of particles, ISO 18562-2 includes a guide for converting this count to a total mass based on the density of the materials used in the gas pathways of the device. 3
VOCs. The second major hazard associated with breathing gas pathways of medical devices is VOCs that can be emitted in the gas stream. VOCs are evaluated under Part 3 of ISO 18562. 4 Since ISO 18562-3 does not recommend specific methods for collecting and sampling VOCs, many laboratories have decided to use thermal desorption tubes/canisters for the collection of VOCs emitted from the medical device and thermal desorption GS/MS for the analysis of the VOCs collected.8 Thermal desorption tubes/canisters are packed with mixtures of different carbon-based absorbent materials that are designed to attract and trap VOCs. These tubes/canisters are then transferred to a GC/MS with a thermal desorption unit that heats the tubes/canisters. VOCs by nature become more volatile at higher temperatures, allowing them to desorb from the absorbent material and enter the equipment for analysis. 8 Since higher temperatures increase the volatility of VOCs, during testing the medical device must be maintained at its highest rated ambient temperature as this allows for the most VOCs to be emitted. 4
Leachables. The final hazard specific to the gas pathway of medical devices is addressed in Part 4 of ISO 18562. This section of the standard outlines the testing requirements for leachables in condensate. 5 This becomes important for devices that deliver humidified gas; where the gas pathway can reach 100 percent saturation with water, condensation can form in the gas pathway of the device, and that condensate can reach the patient. ISO 18562-4 requires that leachables in the condensate be evaluated for all of devices that meet these conditions. 5 This part of the standard suggests three methods for collecting these leachable substances:
Use clinical conditions to cause the formation of condensation in the gas pathway,
Circulate water through the gas pathway in conditions similar to clinical use, or
Perform an aqueous extraction 5 according the principles established in ISO 10993-129.
All three of these methods are sufficient to collect any hazardous leachables that may be present in condensation that develops during clinical use.
Once the condensation has been generated and collected or the aqueous extract collected, ISO 18562-4 requires analysis and identification of any leachable compounds that are found. ISO 18562-4 specifies that the metal ion concentrations in these samples should be determined using pharmacopeia methods and also any organic impurities quantified and identified using GS/MS5.
Although it is not specifically mentioned in ISO 18562-4, many laboratories also recommend quantifying and identifying less volatile compounds using LC/MS. Importantly, if the materials within the gas pathway of the device have previously been evaluated according to ISO 10993-12, testing according to ISO 18562-4 is not necessary. 5
Toxicological Evaluation
Following the emission testing outlined in ISO 18562, the chemical compounds identified in Parts 3 and 4 of ISO 18562 must undergo a full toxicological evaluation according to ISO 10993-17. 10 The first step in this evaluation is to calculate the actual dose of the identified compounds to the patients. This includes considering parameters such as dilution from the amount of gas and the breathing volume of the target patient population. 2 Once a dose to the patient is established for each compound, an extensive literature search of all available toxicological data and derivation of allowable daily limits for each compound can be performed. It is important that toxicologists pay extra attention to available inhalation toxicity data as this data will be the most relevant to breathing gas pathways. If there are any compounds that are found to pose a toxicological concern to patients, ISO 18562 recommends performing cytotoxicity and sensitization testing according to ISO 10993-5 and -10, respectively. 11, 12
Once all of this information and data is collected, the acceptability of the breathing gas pathway device can be sufficiently determined.2 With that being said, the medical device must be evaluated in total. No single test or evaluation is adequate to evaluate a medical device. Instead, it is the consideration of all the test data and toxicological information that allows regulatory bodies to adequately determine the safety of a breathing device.
Conclusion
It is important to remember that this is the initial release of a new international standard. As data is generated and experts continue to weigh in, ISO 18562 will continue to evolve until it is the preferred standard by regulatory bodies worldwide. While ISO 18562 is not currently on the FDA’s list of Recognized Consensus Standards, many reviewers will still ask for the tests outlined in ISO 18562. 13
These requests foreshadow the shift in perspective toward the eventual adaptation of this standard as it is revised and enhanced. Therefore, understanding the testing requirements of ISO 18562 will help to ensure a complete regulatory submission and save valuable resources when working to get a medical device to market.
This article was written by James Lyons, PhD, Toxicologist for Eurofins Medical Device Testing, Lancaster, PA. For more information, visit here .



