While technological advancements continue to enable medical devices to become more capable and more compact, the use of advanced electronics has also created thermal management issues. Laser diodes, LEDs, transistors, transducers, electrodes, motors, and other advanced electronics increase heat loads in handheld surgical instruments, imaging machines, diagnostic equipment and many other medical devices.
As a result, medical device manufacturers must meet strict standards to ensure that their devices do not unintentionally harm patients or care providers (in accordance with IEC 60601). In addition, thermal devices used to manage the temperature of patients must adhere to strict safety, reliability, and temperature control requirements (IEC 80601 & ASTM F2196-02).
While designers of electronically intensive devices face the challenge of dissipating heat more effectively, they must also deal with a specific bioburden known as fouling. Biofouling occurs when pathogens are allowed to collect in a given area that is not disinfected and could expose humans to infection risks. A significant competitive advantage could be obtained by medical device original equipment manufacturers (OEMs) who can offer devices that address both touch temperature and hygiene challenges.
Hygienic design is especially important given recent efforts to reduce hospital- acquired infections (HAIs). According to the U.S. Centers for Disease Control and Prevention (CDC), HAIs cost the healthcare system more than $25 billion in treatment per year.
The CDC has recently sponsored programs to improve staff awareness and cleaning methods in healthcare facilities. Medicare is also incentivizing hospitals to take action by penalizing those with infection rates above the allowable limits. The improved cleaning regiments appear have been effective, since mortality rates in the US have dropped from 100,000 to 75,000 per year. However, it is also important to consider the design of medical equipment itself—especially devices that use fans and heat sinks, which can collect and distribute pathogens.
Focusing on Hygienic Equipment Design
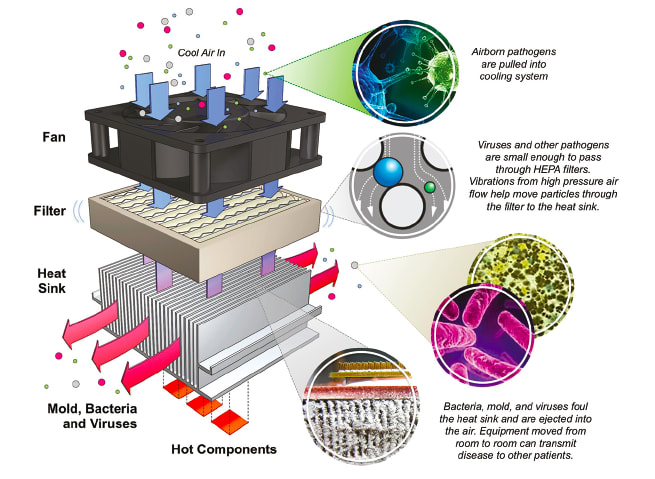
Devices employing fan-cooled heat sinks can collect and transmit bacteria and viruses. HEPA filters are sometimes used to remove airborne pathogens that pass through heat sinks in medical devices. These filters are assumed to be impermeable to microbes since they have the ability to capture 99.97 percent of particles that are 0.3 microns in size. However, the manufacturers of these types of filters make no claims for particles smaller than this, since their efficiencies are dependent on airflow velocity and pressure. These filters rely on diffusion to capture particles below 0.2 microns. (See Figure 1)
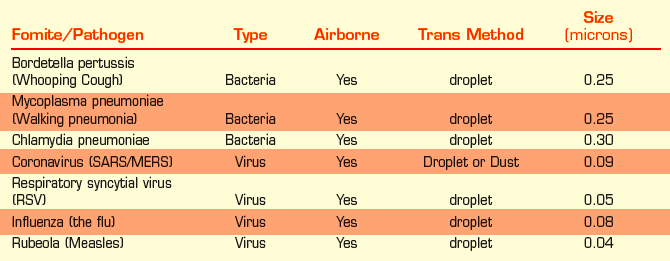
The effectiveness of most filter capture methods decreases as airflow velocity increases, especially for the diffusion capture method. In addition, as airflow velocity increases, airborne droplets that contain pathogens break into smaller droplets and can even disagglomerate microbes that are bound together. This enables the pathogens to penetrate the filter and potentially infect people that are in proximity of the device. (See Table 1)
In the past, it was assumed that airborne transmission was limited to just a few feet. However recent studies have shown that airborne microbes can travel much further distances.
Understanding the Role of Thermal Management Technology in Hygiene
To dissipate heat from medical devices, medical device OEMs employ a variety of thermal management solutions that primarily fall into two categories: active and passive technologies. Most active cooling systems utilize forced air convection by incorporating fans that direct air through aluminum heat sinks. These components can function as fomites, surfaces that harbor viral and bacterial pathogens associated with HAIs. The airflow can eject these pathogens into the air and infect new patients, especially when these devices are moved from room to room. Unfortunately, many hospitals are still unaware of how fans within a device can contribute to HAIs.
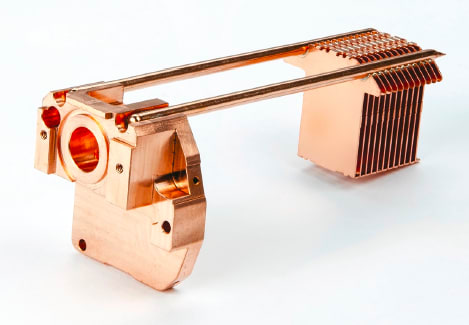
In contrast, passive thermal management solutions use technologies that can reduce infection vector potentials. By definition, passive components have no moving parts and do not require a power source. Optimized thermal management systems can reduce airflow requirements to improve filter efficiency, thus reducing the bioburden associated with pathogens that can pass through medical device cooling systems. Passive technologies include heat pipe assemblies and vapor chambers, as well as the use of Annealed Pyrolytic Graphite (APG) components, which do not require fans or pumps.
Passive heat spreaders quickly transfer heat from concentrated, high-heat flux (W/cm2) sources inside the device to external heat sinks, remote liquid cooling lines or even to the outer wall of the enclosure. This isolates the interior of the device from the environment, eliminating the flow of air and microbes inside the device. The external components can be easily cleaned with disinfectants or even with UV light systems to prevent biofouling. Heat sinks can also be composed of or plated with antimicrobial materials.
Heat Pipes
Heat pipes transfer high heat loads in small spaces. The majority of heat pipes consist of metal tubes with sintered powder wicks that line the inner walls. A vacuum is pulled inside the vessel and a small amount of working fluid is inserted before it is sealed. As heat enters one or more points on the tube, the working fluid evaporates and the vapor quickly travels through the vacuum until it reaches a cooler region where it condenses into a liquid. The wick structure then transports the liquid back to the heat source and this phase change cycle continues perpetually. Some heat pipes have been undergoing continuous life testing for more than 45 years.
Heat pipes can be designed to operate in a variety of temperature ranges, ranging from -265°C to 2,200°C. Heat pipes can be less than 2 mm in diameter, can be formed to fit in complex geometries, and can even be made flexible. They offer thermal conductivities that increase with length and are many orders of magnitude higher than solid copper.
As a rule of thumb, designers should assume a minimum bend radius of three times the heat pipe diameter. Another design consideration is that heat pipes have an inactive region on one side that ranges from 4 mm to 12 mm depending on the diameter, material, and manufacturer. This is created when the sealing operation fills in the vapor space in that area, leaving only solid conduction. It is usually best to position this inactive region on the heat sink side of the heat pipe, where there is usually more space available and the heat fluxes tend to be lower.
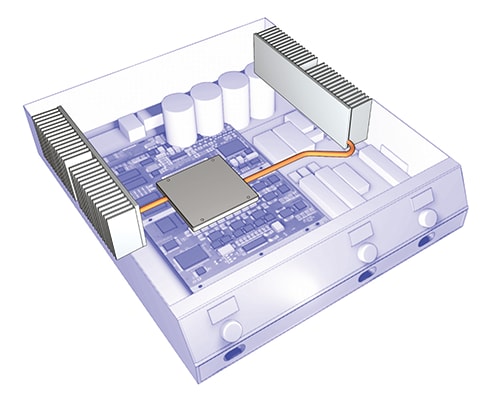
Heat pipes are often used to spread heat across the base of heat sinks to make them more efficient, which reduces the amount of airflow required and can even eliminate the need for a fan by optimizing natural convection. (See Figure 2)
Vapor Chambers
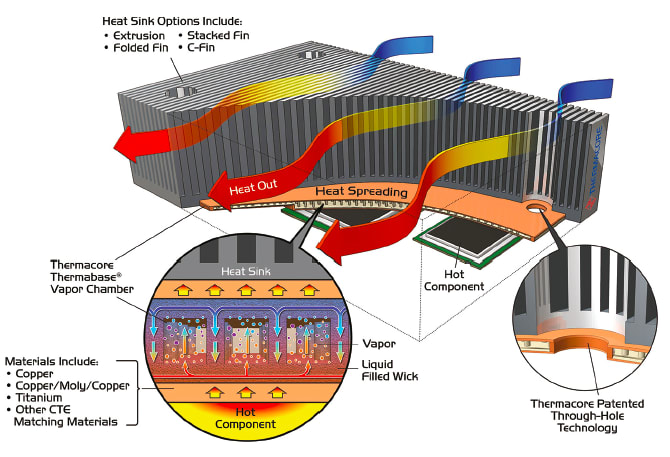
Vapor chambers are planar (flat) versions of heat pipes. Vapor chambers are evacuated vessels with a small amount of working fluid inside and a capillary wick structure that lines the internal surfaces. Vapor chambers provide excellent heat spreading capability in all directions and can dissipate high heat fluxes with rapid thermal cycling. Vapor chambers can be designed to be less than 1 mm thick. For some applications, they can be matched to the coefficients of thermal expansion (CTE) of mating components to allow for direct-die-attach to electronics. These Thermal Ground Plane (TGP) vapor chambers eliminate the need for substrates, making them ideal for medical devices that require compact configurations. (See Figure 3)
Annealed Pyrolytic Graphite
Annealed Pyrolytic Graphite (APG) is an advanced solid conduction material that is ideal for medical applications. APG can be encapsulated with many different biocompatible materials. APG is lightweight—20 percent lighter than aluminum. It has high thermal conductivity—up to 4x the thermal conductivity of copper and 6x the conductivity of copper at cryogenic temperatures. It enables a solid-state design that exhibits consistent performance, regardless of gravity, giving designers considerable flexibility in creating medical device solutions.
Conclusion
As a category, passive thermal technologies that require less airflow give designers a number of advantages, which include:
- Lower noise levels,
- Smaller package sizes or weights,
- Reduced healthcare associated infection risks,
- Extended duty cycles and component lives, and
- Improved isothermality levels to meet precise instrument requirements.
Choosing the optimum thermal management solution that addresses both thermal and hygiene issues requires a detailed understanding of the capabilities and limitations of specific thermal management technologies. The advantages of passive thermal management solutions can help designers create devices that minimize the possibility of HAIs while providing the safety and reliability required in today’s electronically intensive medical devices. (See Figure 4)
This article was written by Michael Bucci, Market Development Manager, Thermacore Inc., Lancaster, PA. For more information, Click Here .



